If the last decade was about collecting patient data, 2025 is about making it work — across systems, teams, and even countries.
Healthcare interoperability isn’t just a regulatory checkbox anymore. It’s becoming the invisible engine behind smarter decisions, faster treatments, and better patient experiences.
Let’s rewind just a few years.
Sure, health systems were exchanging data, but not in a way that truly helped patients or providers in real-time.
Updates were processed in batches, often overnight.
Was a referral sent on Monday? It might show up in the EHR by Thursday.
A medication history? Someone could fax it if you were lucky.
This was the batch era — disconnected, slow-moving, and often riddled with blind spots.
But something is changing.
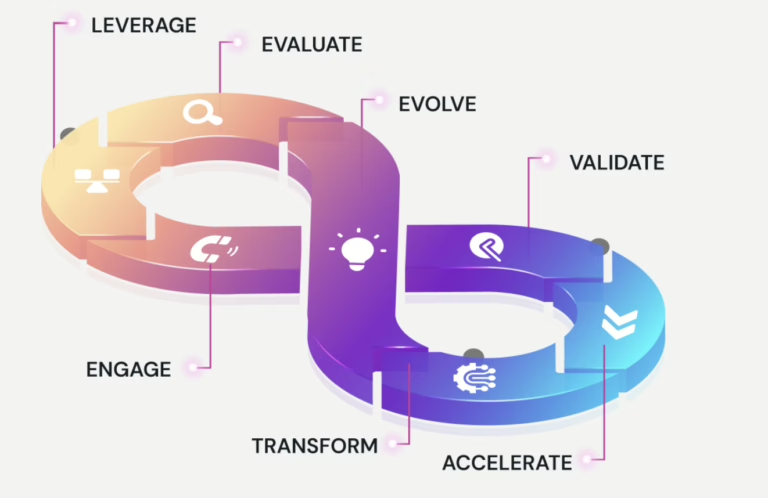
Today, the U.S. healthcare system is moving toward an impact-driven model of interoperability — where information isn’t just exchanged, it’s immediately actionable.
We’re talking:
- Prior auth decisions are made in minutes — not weeks.
- Lab results auto-syncing across systems during a patient visit.
- Smart alerts surfacing critical history before a prescription is written.
- Interoperability is no longer an IT initiative parked in the basement.
It’s now a frontline enabler — influencing clinical decisions, improving care coordination, and, yes, reducing burnout.
This shift—quiet, foundational, and deeply transformative—is driving every major trend in modern healthcare tech.
Let’s break them down.
1. FHIR + TEFCA: Finally Talking to Each Other
For years, FHIR sat in development rooms, and TEFCA lived in policy papers. Now, they’re finally showing up where it matters — in real-time patient care.
- Hospitals are pulling up external patient records without logging into five systems
- Networks are syncing faster without the “request sent, please wait” cycle
- Clinicians are seeing the bigger picture — allergies, meds, history — right in their workflow
Why it matters: This isn’t about standards on paper. It’s about a cancer specialist having a complete picture before prescribing that next dose.
2. Interoperability is Smarter Now — Thanks to AI
AI is no longer just for imaging or diagnosis. It’s also helping to clean up the mess in health records.
- NLP tools are turning scribbled notes into structured insights
- AI bots are spotting duplicate entries, outdated allergies, or missing data
- Live patient data is flowing into predictive models to catch risks before they escalate
What’s new: It’s not just “data exchange” — it’s “data that makes sense, right now.”
3. Prior Authorization: No Longer a Black Hole
Let’s be honest — prior auth has always been the slowest part of the system. But that’s changing.
- New APIs are cutting approval times from days to minutes
- Some pilot programs are seeing 60% fewer manual reviews
- Docs are spending more time with patients, not fax machines
The shift: This isn’t just process improvement — it’s giving clinicians their time (and sanity) back.
4. Security Is Not an Afterthought Anymore
With breaches hitting the headlines every month, healthcare organizations are done treating security like a “later” problem.
- Networks are getting smarter at spotting weird access patterns
- Zero-trust setups are becoming the default, not deluxe
- Interoperability layers now come with built-in protection — not patched-in firewalls
The bottom line: If data can move, it better be locked down every step of the way.
5. EHDS Is Making Everyone Rethink Patient Data
The European Health Data Space isn’t just a local regulation — it’s making global systems take notice.
- Patients can now carry and control their records across borders
- Researchers can access population data without fighting red tape
- Health systems are being held to higher transparency standards
Why it matters: This is the start of patient-owned health data, not just provider-managed files.
6. Remote Monitoring: The Real Interoperability Test
Devices are everywhere — glucose monitors, smartwatches, heart patches. The question is: can they talk to the system that actually treats you?
- Vitals from home are starting to ping care teams in real time
- RPM platforms are syncing with hospital EHRs, not just sending PDFs
- Smart alerts are going out before a patient even knows something’s off
Big takeaway: If your data can’t travel with you, it’s not really “care anywhere.”
So, What Now?
This isn’t about future-proofing anymore. It’s about catching up with what patients already expect: connected care that makes sense.
At 47Billion, we’re working with healthcare providers and tech teams to make systems smarter — not just compliant. Whether it’s integrating wearable data into treatment plans, streamlining payer workflows, or helping clinicians see the whole story — we’re in it for the real change.
Want to see what connected care could look like for your system?
Let’s talk: hello@testing-new.47billion.com | www.47billion.com/healthcare