If 2025 is the year interoperability became real, TEFCA is the reason it’s finally becoming reliable.
Healthcare has long been a paradox: cutting-edge inside the OR, but held together by duct tape when it comes to data. We’ve had EHRs, APIs, and a dizzying amount of standards — but until now, we’ve lacked a national framework that aligns technology, policy, and trust.
That’s exactly what TEFCA (Trusted Exchange Framework and Common Agreement) is solving for.
This isn’t just another compliance update — this is a systemic overhaul of how healthcare communicates.
1. TEFCA Isn’t Just About Sharing Data — It’s About Trust at Scale
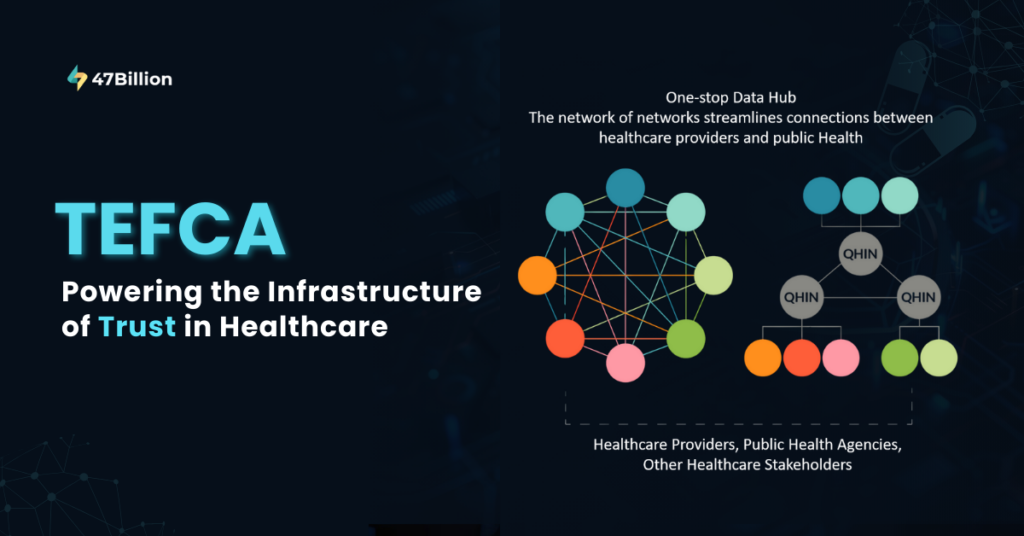
At its core, TEFCA is not a technology product — it’s a governance architecture.
It defines how entities establish trusted connections under a universal agreement, removing the fragmented, one-off connections that slowed down care and broke workflows.
Before TEFCA:
Every integration was a separate legal agreement
Trust was local, not national
Security was optional, not enforced
After TEFCA:
Participants connect once to a QHIN (Qualified Health Information Network) and gain access to a nationwide network
Trust and identity verification are pre-baked into the infrastructure
Data access is policy-aligned, patient-consented, and immediately actionable
It’s the difference between building individual bridges… and having an FAA-level air traffic system.
2. TEFCA + FHIR: The Operating System of Connected Healthcare
FHIR has been around for years — hailed as the answer to data portability. But without a highway to move those packets efficiently, even the best APIs fall flat.
TEFCA provides:
The backbone — trust policies, data-sharing permissions, security frameworks
FHIR provides:
The language — clean, structured, developer-friendly data objects
Together, they finally offer scale + structure — making real-time care coordination the default, not the exception.
3. The QHIN Era: Simplifying Complexity for Providers and Payers
Qualified Health Information Networks (QHINs) are the engine rooms of TEFCA. Once a provider or payer connects to a QHIN, they are essentially connected to all other networks within the TEFCA ecosystem — with no new contracts, no fresh integrations.
What does this mean for health systems?
Instant data liquidity — referral records, imaging, prior histories all travel instantly
Reduced duplicative testing — real-time access to external labs
Improved transitions of care — no more patients acting as data couriers
Payer-provider alignment — eligibility, prior auth, and medical necessity data is aligned at the source
It’s not just interoperability. It’s intelligent, consent-driven, and context-aware connectivity.
4. The Operational Shift: From IT Projects to Clinical Enablement
TEFCA’s greatest contribution might be cultural, not technical. It shifts interoperability from an IT department burden to a core clinical enabler.
Emergency rooms access critical history without delay
Chronic care teams see medication adherence from external systems
Behavioral and physical health records are finally integrated
This shift reduces:
Clinician burnout (by cutting screen time and system switching)
Medical errors (through full-context decision-making)
Delays in treatment (because information arrives with the patient, not after them)
TEFCA is not an update. It’s a new layer of healthcare delivery.
Interoperability is Smarter Now—Thanks to AI
AI is no longer just for imaging or diagnosis. It also helps clean up the mess in health records.
Natural Language Processing (NLP) tools are turning scribbled notes into structured insights. AI bots are spotting duplicate entries, outdated allergies, or missing data. Live patient data is flowing into predictive models to catch risks before they escalate.
It’s not just “data exchange”—it’s “data that makes sense right now.”
Prior Authorization: No Longer a Black Hole
Prior authorization has always been the slowest part of the system. But that’s changing.
New APIs are cutting approval times from days to minutes. Some pilot programs are seeing 60% fewer manual reviews. Doctors are spending more time with patients, not fax machines.
This isn’t just process improvement—it’s giving clinicians their time (and sanity) back.
Security Is Not an Afterthought Anymore
With breaches hitting the headlines every month, healthcare organizations are done treating security like a “later” problem.
Networks are becoming more competent at spotting unusual access patterns. Zero-trust setups are becoming the default, not deluxe. Interoperability layers now come with built-in protection, population data without fighting red tape, and health systems are being held to higher transparency standards.
This is the start of patient-owned health data, not just provider-managed files.
not patched-in firewalls.
If data can move, it better be locked down every step of the way.
EHDS Is Making Everyone Rethink Patient Data
The European Health Data Space (EHDS) isn’t just a local regulation—it’s causing global systems to pay attention.
Patients can now carry and control their records across borders, researchers can access
Remote Monitoring: The Real Interoperability Test
Devices are everywhere—glucose monitors, smartwatches, heart patches. The question is – Can they talk to the system that actually treats you?
Vitals from home are starting to ping care teams in real-time. Remote Patient Monitoring (RPM) platforms are syncing with hospital EHRs, not just sending PDFs. Smart alerts are going out before a patient even knows something’s off.
If your data can’t travel with you, it’s not really “care anywhere.”
5. What’s Next: TEFCA Is Only as Powerful as the Experiences Built on Top
The framework is robust, but the real innovation lies in how healthcare organizations use it. At 47Billion, we’re seeing forward-thinking partners already build on TEFCA infrastructure by:
Embedding FHIR-enabled decision support in clinical workflows
Designing real-time, cross-network patient summary views
Creating interoperability dashboards that provide actionable visibility, not just data dumps
Streamlining prior authorization with EHR-integrated TEFCA queries
This is where compliance turns into competitive advantage.
6. The Clock Is Ticking: Early Adoption Means Early Impact
The window is narrow. Early TEFCA adopters aren’t just checking boxes — they’re setting new standards for patient experience, clinician efficiency, and data governance.
For executives, this means:
Aligning your EHR roadmap with TEFCA integration timelines
Prioritizing partnerships with QHINs that suit your regional and specialty needs
Rethinking patient data strategy as network-first, not system-first
Partnering with experienced interoperability experts to build your application layer
Final Word: This Isn’t a Tech Trend — It’s the New Baseline
TEFCA won’t make headlines. But it will change the foundation of how U.S. healthcare works.
It’s not about hype. It’s about infrastructure-level change.
And for those ready to lead — not just adapt — this is the moment to architect something truly future-ready.
Let’s make connected care real — with trust, security, and clinical purpose.
📩 hello@testing-new.47billion.com 🌐 www.47billion.com/healthcare